What Is a Medicare SNP and How Does It Work?
Medicare SNPs (Special Needs Plans) have coverage focused on specific health care needs like kidney failure or needing long-term care.
Compare Medicare Plans in Your Area
You may be able to get an SNP if you live with a chronic or debilitating health condition, need nursing home care or are eligible for both Medicare and Medicaid.
What is a Medicare SNP?
A Medicare Special Needs Plan (SNP) is a type of Medicare Advantage plan built for those with specific health care needs.
Also called Medicare Part C plans, Medicare Advantage plans bundle Medicare Parts A and B together and usually include prescription drug coverage. Plans come from private insurance companies, not the government.
For example, you can only get an SNP for people with end-stage liver disease if you have that condition. The plan's network probably includes doctors who specialize in end-stage liver disease, and the covered medications likely also include drugs used to treat liver disease. Some SNPs also give you access to professionals who help you navigate your coverage and treatments, called care coordinators.
There are three types of Special Needs Plans:
- C-SNPs are for people who have chronic or severe health problems, like cancer, dementia or certain lung disorders. About 8% of people with an SNP have a C-SNP.
- D-SNPs are for people who can get both Medicare and Medicaid, called being "dual qualified." These plans can help coordinate coverage between the two programs. Nearly 90% of people in an SNP are in a D-SNP.
- I-SNPs are for people who live or who expect to live in a care facility like a rehab hospital or nursing home for 90 or more days in a row or people who live outside a facility but need the same level of care. I-SNPs are the least common plan type. Less than 2% of people with an SNP have an I-SNP.
Not everyone who can get Medicare can get an SNP. But if you can get a Special Needs Plan, you'll probably get coverage that is better for your unique needs.
Pros and cons of SNPs
Pros
-
Coverage based on your health needs
-
Help managing your treatment
-
Rates can be low
Cons
-
Availability depends on where you live
-
Requires you to use certain doctors
-
May need a referral to see a specialist
How much do SNPs cost?
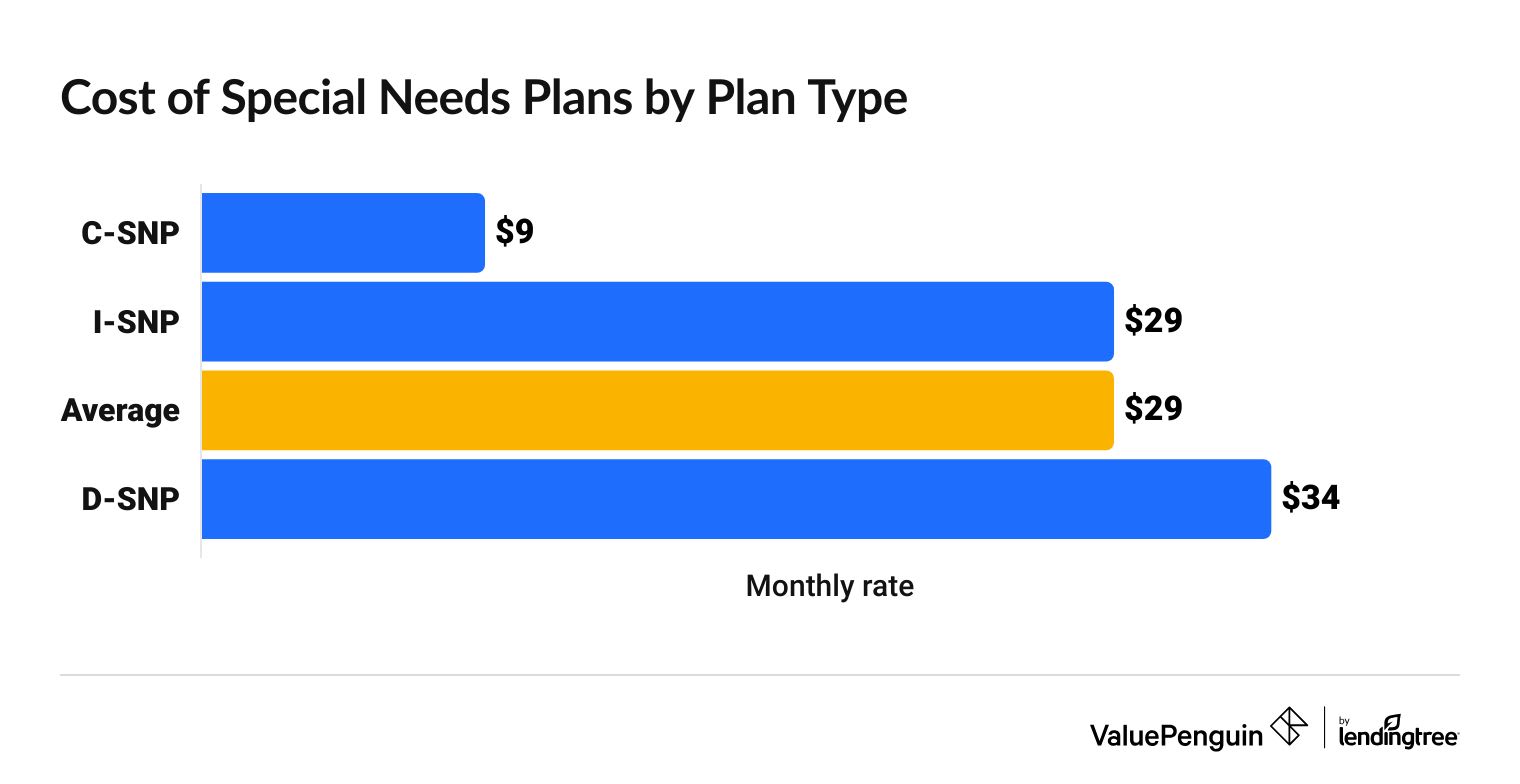
On average, SNPs cost $29 per month.
The cost changes depending on the type of SNP you get. C-SNPs tend to have the cheapest rates, at an average of $9 per month. D-SNPs are the most expensive, costing $34 per month, on average.
Compare Medicare Plans in Your Area
Cost of SNPs by plan type
SNP type | Monthly rate |
|---|---|
| C-SNP | $9 |
| I-SNP | $29 |
| D-SNP | $34 |
Keep in mind, you'll also have to pay for Medicare Part B on top of your monthly rate for the SNP.
Medicare Part B costs $185 per month in 2025. However, if you earn more than $106,000 per year, you'll pay more.
Medicare Part A is free for most people. And all SNPs include Part D, which covers prescriptions, so you won't pay anything extra for drug coverage.
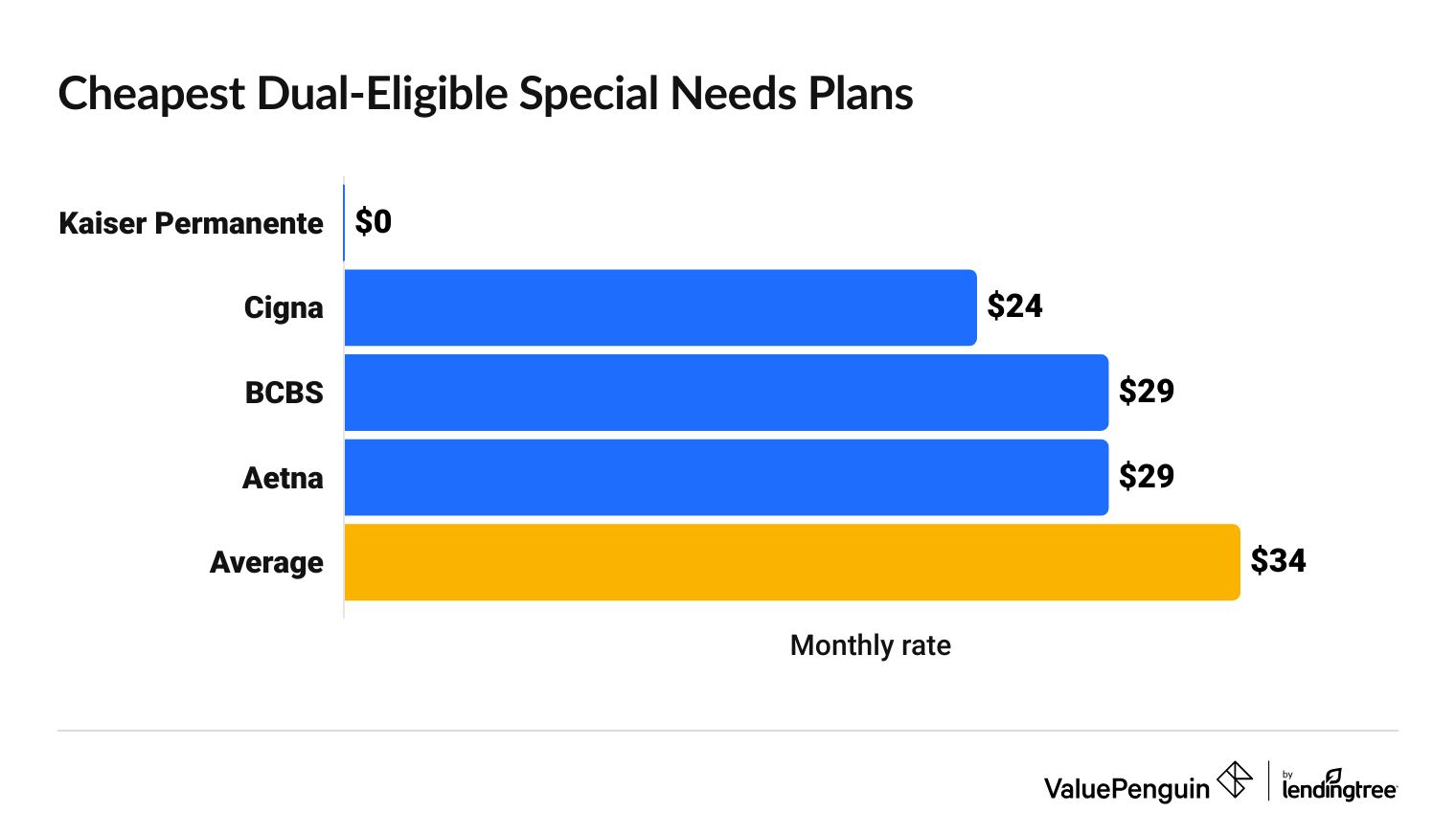
D-SNP costs
Kaiser Permanente has the cheapest average D-SNP rates. Most of its plans have no monthly cost.
Compare Medicare Plans in Your Area
D-SNPs are the most common type of Special Needs Plan. About 90% of people with an SNP have a dual-eligible plan. That's over 5.6 million people.
D-SNP rates by company
Company | Monthly D-SNP rate | |
|---|---|---|
| Kaiser Permanente | $0 | |
| Cigna | $24 | |
| Blue Cross Blue Shield | $29 | |
| Aetna | $29 | |
| Centene | $37 | |
Centene includes Allwell and Wellcare plans.
D-SNP rates by state
California, New Mexico and Texas have the cheapest average rates for D-SNPs, at $14 per month.
D-SNPs are most expensive in New York, where the average rate is $56 per month.
While D-SNPs are widely available, no companies sell plans in Alaska, Illinois, New Hampshire or Vermont.
Compare Medicare Plans in Your Area
What do SNPs cover?
SNPs cover everything that other Medicare Advantage plans cover and may have additional benefits.
Medicare Advantage plans bundle together coverage for Medicare Part A, which covers medical care in hospitals, and Medicare Part B, which covers things like doctor visits and medical tests that happen outside the hospital.
While not all Medicare Advantage plans include Medicare Part D, which covers prescription medications, all Special Needs Plans are required to include it.
Because SNPs are designed for specific groups of people, they might also include additional coverage perks, like higher limits for hospital stays. Many SNPs also include dental and vision coverage.
How to apply for Special Needs Plans
If you're already covered by Medicare, you can usually join an SNP at any time, as long as you qualify.
Developing a condition, needing nursing home care or qualifying for both Medicare and Medicaid usually allows Medicare enrollees to get an SNP at any time because these are considered "special enrollment" situations.
To join an SNP, you'll first need to be eligible for Medicare. Medicare Parts A and B have three enrollment periods, or periods of time when you can sign up for coverage.
- Initial enrollment: This is the most common time to enroll in Medicare and generally happens when you turn 65, although you may qualify for Medicare earlier if you have a disability, kidney failure (ESRD) or Lou Gehrig's disease (ALS). If you qualify because of your age, your initial enrollment period begins three months before the month you turn 65 and ends three months later, so you have a total of seven months to enroll.
- General enrollment: If you don't sign up during your initial enrollment period, you can sign up between Jan. 1 and March 31 of every year. However, you may pay a penalty unless you qualify for special enrollment.
- Special enrollment: In some circumstances, you can sign up for Medicare Parts A and B outside of the initial and general enrollment periods without paying a late penalty. These include missing your chance to sign up due to a natural disaster, incorrect information from a health plan or employer, or volunteering or serving in another country.
As you're looking for coverage, remember that SNPs are sold by insurance companies and don't come directly from the government. You can compare plans on Medicare.gov or reach out to a company directly.
Frequently asked questions
What are the three types of Medicare Special Needs Plans?
The three types of SNPs are Chronic Condition SNP (C-SNP), Dual-Eligible SNP (D-SNP) and Institutional SNP (I-SNP). Each plan type is designed for a specific group of people. Only people who can get both Medicare and Medicaid can join D-SNPs. Only people with certain chronic illnesses can get a C-SNP, and only people who need long-term care can get I-SNPs.
How do you qualify for a D-SNP?
To get a D-SNP, you have to have both Medicare and Medicaid coverage. For most people, this probably means being 65 or older and making less than $21,597 per year. If you qualify, you can compare D-SNPs on Medicare.gov and choose one that works for you.
What chronic conditions qualify for an SNP?
Conditions like asthma, cancer, dementia, major depressive disorder, alcohol or drug dependence and chronic heart failure all mean you can get a C-SNP.
Methodology
Medicare SNP costs come from public use files (PUFs) on the Centers for Medicare & Medicaid Services (CMS) government website. Rates are based on 2025 Medicare Advantage Special Needs Plans and include drug coverage. This analysis excludes employer-sponsored plans, sanctioned plans and state-specific Medicare-Medicaid Plans (MMPs). Info about the number of people in D-SNPs comes from the CMS SNP Comprehensive Report from October 2023.
Insurance Writer
Cate Deventer is a ValuePenguin writer who specializes in health insurance, Medicare, auto and home insurance. She's been a licensed insurance agent since 2011.
She started her insurance career working as a customer service agent for State Farm. She later moved to an independent agency, where she worked with several insurance companies and hundreds of clients. She quoted policies, filed claims and answered insurance questions. In 2021, she pivoted her career and began writing about insurance for Bankrate. She moved to ValuePenguin in 2023 and began writing about health insurance and Medicare.
Cate has a passion for helping readers choose insurance to fit their needs. She enjoys knowing that her research and knowledge help people choose insurance products that make a positive difference in their lives.
How insurance helped Cate
Cate used her health insurance knowledge to navigate a surgery in 2023. Understanding how her policy worked let her focus on recovery instead of worrying about bills.
Expertise
- Health insurance
- Medicare & Medicaid
- Auto insurance
- Home insurance
- Life insurance
Credentials
- Licensed Life, Accident & Health Insurance Agent
- Licensed Property & Casualty Insurance Agent
Referenced by
- CBS
- NBC
- Wall Street Journal
Education
- BA, Theatre, Purdue University
- BA, English, Indiana University
Editorial Note: We are committed to providing accurate content that helps you make informed financial decisions. Our partners have not endorsed or commissioned this content.





