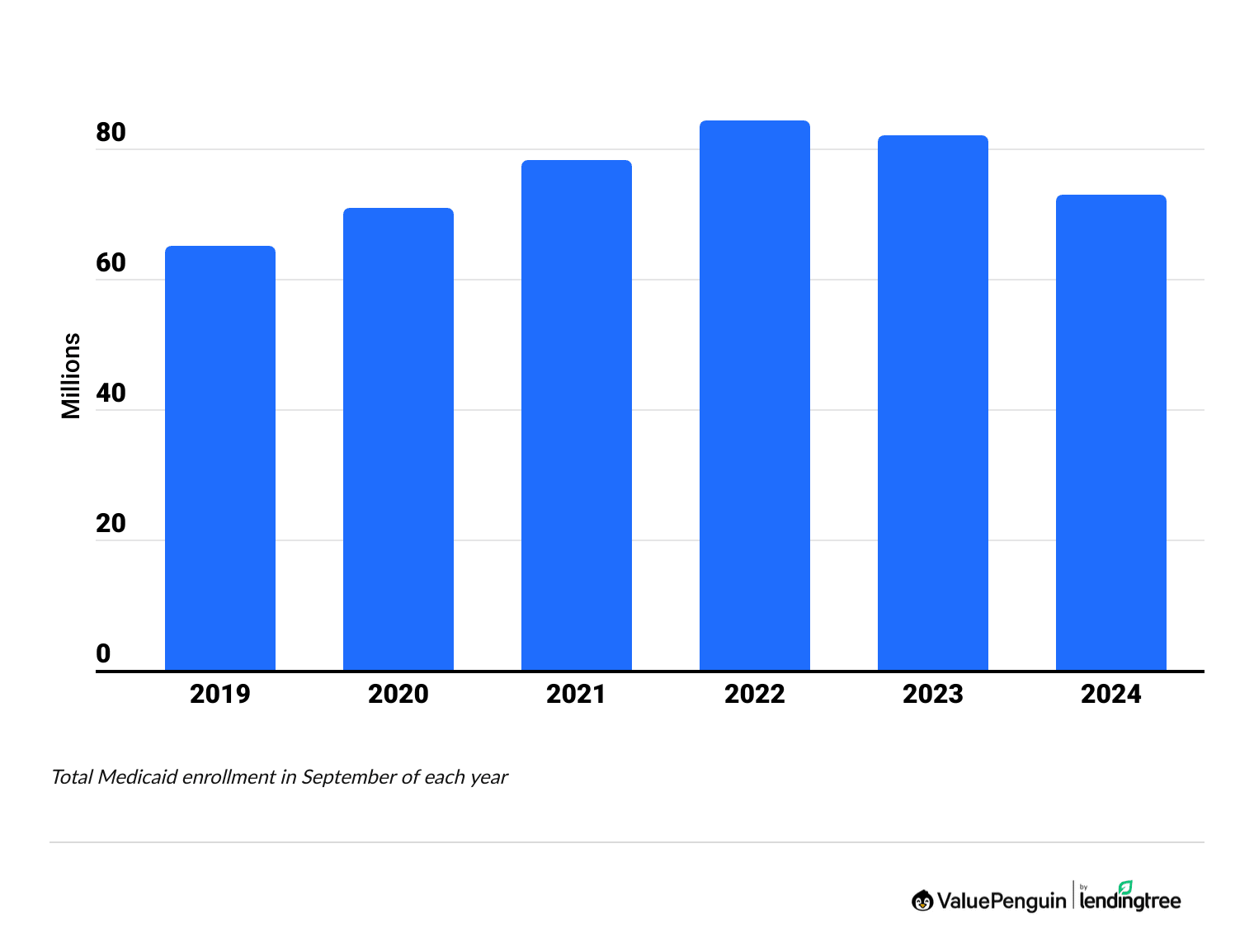
How Has Medicaid Enrollment Changed?
About 80 million people had Medicaid or CHIP in the fall of 2024. That's 11% less than 2023.
How many people are on Medicaid?
There are almost 72.7 million people with Medicaid and over 7.2 million people with CHIP coverage in the U.S.
Since Medicaid unwinding, which meant you had to reapply for coverage, began in March 2023, Medicaid enrollment has gone down by nearly 14.5 million people.
Is Medicaid changing in 2025?
As of June 2025, Medicaid has not changed. However, there are potential new rules being considered in the Senate that could impact how many people can get Medicaid. If you're on Medicaid, keep an eye on the news and talk to your state's Medicaid office if you're concerned or confused about your coverage. Keep in mind that each state has some ability to regulate its own Medicaid program, which means enrollment requirements vary depending on where you live.
Earlier this year, the Medicaid portal experienced an outage. However, as of Wednesday, Jan. 29, access has been restored.
Potential changes to Medicaid are developing. More information will be added as it becomes available.
Last updated June 10, 2025
On this page
Medicaid enrollment changes
In the past year, Medicare enrollment went down by 11% nationally.
The largest declines were in Colorado, Michigan, Mississippi and New Jersey, where Medicaid enrollment fell by 20% to 28%.
North Carolina, South Dakota, Alaska and Idaho saw increases in Medicaid enrollment in 2024.
Medicaid enrollment by state
Why Medicaid enrollment declined last year
Last year's drop in Medicaid enrollment is largely because of a policy change that forced many people to re-apply for Medicaid. In 2023, a pandemic policy ended, and it resulted in many people losing coverage. This is called Medicaid unwinding, and it continued throughout 2024.
How has Medicaid enrollment changed since 2020?
Over the last few years, Medicaid enrollment has increased in some states.
Since 2020, North Carolina's Medicaid enrollment has grown by 47%. That's because North Carolina expanded its Medicaid program in December 2023, allowing more people to qualify based on their incomes.
Medicaid enrollment has also grown by 20% or more in Nebraska, Oklahoma, Missouri, Maine and South Dakota.
What is Medicaid?
Medicaid provides free or low-cost insurance for people who have low incomes, disabilities or substance abuse disorders. That's different from Medicare which covers seniors who are older than 65 and those with a disability.
In many states, you're eligible for Medicaid if you're an individual earning less than about $21,597 per year. That's less than about $44,367 for a family of four. However, the income limit is lower in states that don't meet the national standards of the Affordable Care Act (ACA).
CHIP health insurance enrollment changes
Enrollment in CHIP (Children’s Health Insurance Program) stayed about the same between 2023 and 2024.
At a national level, CHIP enrollment has been mostly stable over the past few years compared to the large swings that Medicaid has had.
However, some states have had large changes in CHIP enrollment. Since 2020, CHIP enrollment has fallen by about 40% in Texas and Oklahoma and has more than doubled in Minnesota and Missouri.
CHIP enrollment by state
Why CHIP enrollment changes
A rise in CHIP enrollment may be tied to changes in the economy, such as people losing their jobs. It could also be related to many people losing Medicaid coverage. Families who earn too much to qualify for Medicaid may enroll their children in CHIP.
What is CHIP?
CHIP provides health insurance to children in families who earn too much to qualify for Medicaid but earn too little to afford private health insurance. In some states, CHIP also covers those who are pregnant and have a low income.
Where you live, and sometimes your child's age, determine how much you can make and still qualify for CHIP. Sometimes, you could make more than three times the federal poverty level and still qualify. That's about $63,450 per year for a single parent with one child or $96,450 per year for a family of four. However, eligibility varies widely by state.
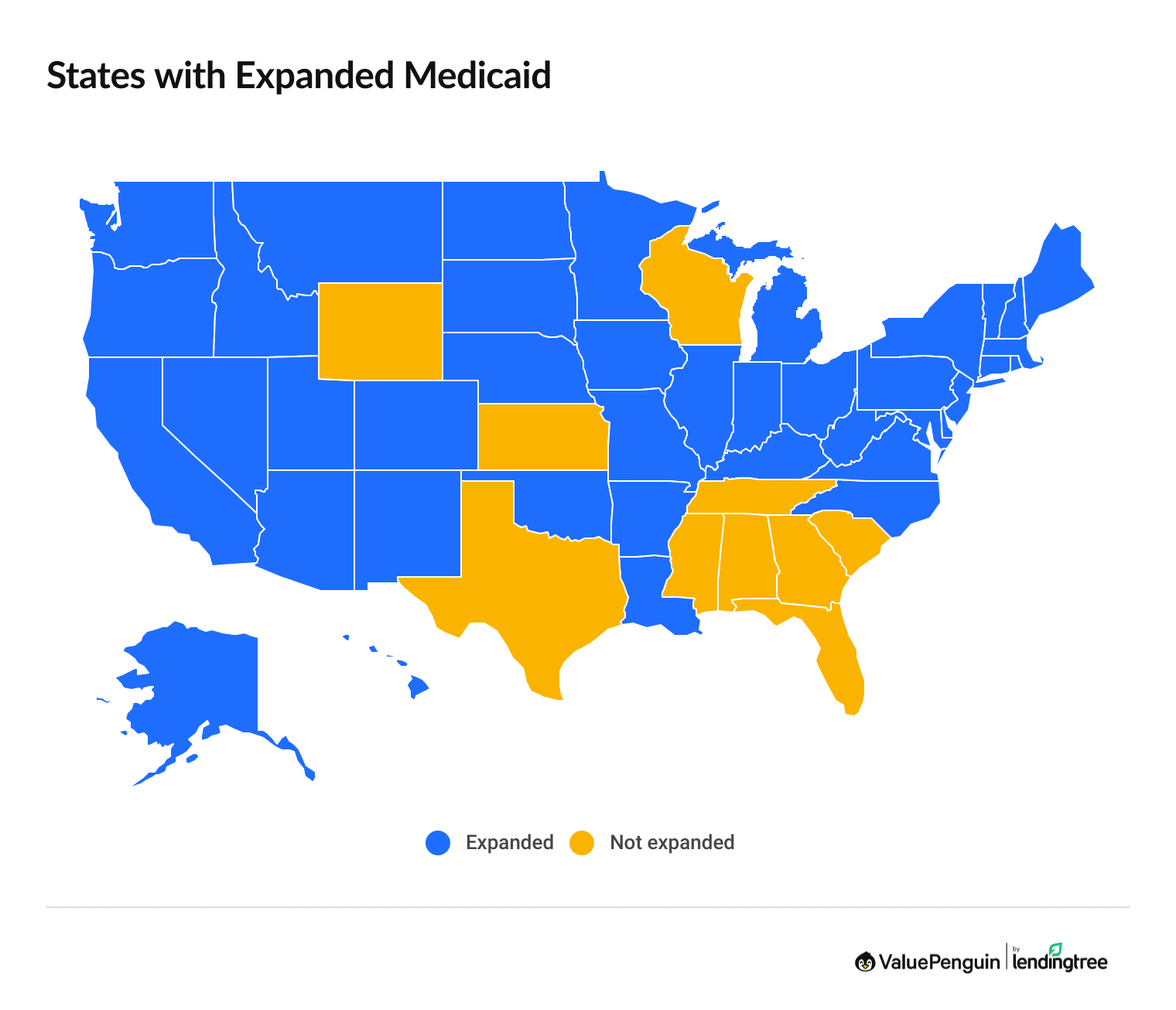
Medicaid expansion
Medicaid eligibility has been expanded in 41 states and Washington, D.C.
Most states have chosen to expand who qualifies for Medicaid to meet the guidelines of the Affordable Care Act (ACA). That means Medicaid eligibility is set at 138% of the poverty level, rather than states setting their own rules about who qualifies.
More people can get Medicaid in states that have expanded their programs. The only requirement to get Medicaid in an expanded state is income. For example, North Carolina expanded Medicaid in 2023. Since 2020, the state's enrollment has jumped 47%.
Medicaid expansion states
State | Expanded? | When expanded? |
|---|---|---|
| Alabama | ||
| Alaska | 2015 | |
| Arizona | 2014 | |
| Arkansas | 2014 | |
| California | 2014 |
Income criteria in states with expanded Medicaid
In states that have expanded their Medicaid program, you're eligible for Medicaid if you earn up to $21,597 if you're single or up to $44,367 for a family of four.
That's because you can make 38% more than the federal poverty line and still qualify. The income limit can be even higher if you're pregnant, under 18 or have another special situation.
How to afford health insurance if you earn too much to qualify for Medicaid
If you earn too much to qualify for Medicaid, you can get discounted health insurance by shopping through the marketplace. Depending where you live, that could mean shopping on HealthCare.gov or a website run by your state.
If you have a low income, you may be able to get discounts on your rate. Obamacare subsidies lower the cost of insurance based on your income, and many people who have a low income can get a plan for less than $10 per month.
Medicaid eligibility in states that haven't expanded Medicaid
In states that haven't expanded Medicaid, there's a wide range of income requirements, and it can be difficult to qualify.
For example, a family of three can only get Medicaid in Texas if they have an income less than $333 per month, or about $3,998 per year. In most states without expanded Medicaid, adults with a low income don't qualify unless they meet another criteria, like having a disability.
This creates a "coverage gap" where someone can earn too much to qualify for Medicaid and too little to qualify for discounted insurance through the marketplace.
Find Cheap Health Insurance in Your Area
Medicaid unwinding and disenrollment
Medicaid unwinding, also called Medicaid redetermination, means that people with Medicaid need to re-apply to keep their coverage after not needing to re-apply during the pandemic. Unwinding started in March 2023 and is ongoing.
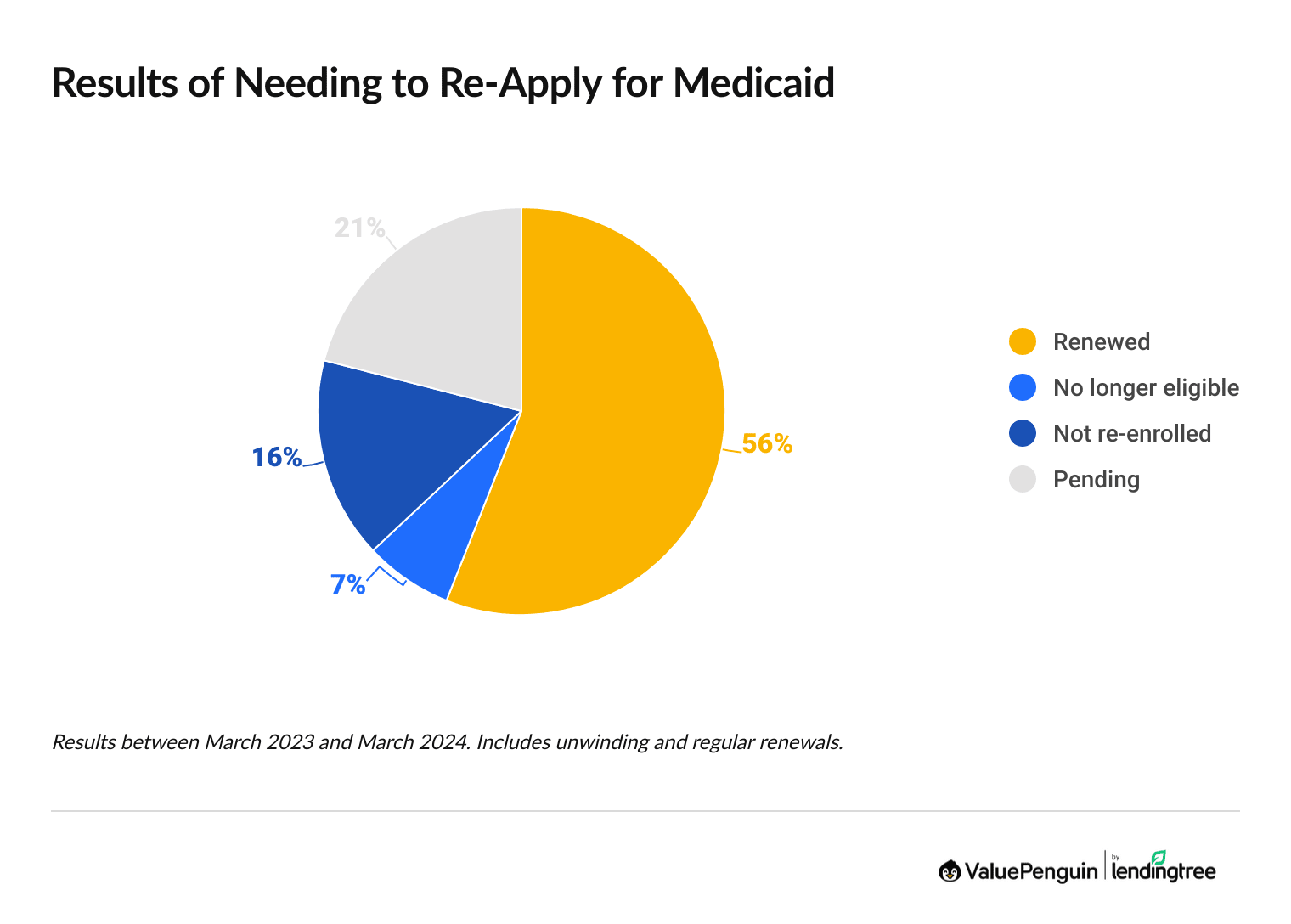
- Between March 2023 and March 2024, about 7% of people who reapplied for Medicaid were found to no longer be eligible.
- About 16% of people had their Medicaid coverage canceled because of administrative reasons such as not reapplying or not having the right paperwork.
Medicaid unwinding results
State | Renewed | Not eligible |
Not re-enrolled
|
|---|---|---|---|
| National | 56% | 7% | 16% |
| Alabama | 65% | 4% | 28% |
| Alaska | 38% | 12% | 15% |
| Arizona | 78% | 5% | 12% |
| Arkansas | 55% | 8% | 27% |
| California | 57% | 2% | 12% |
Totals for March 2023 through March 2024. Data includes unwinding and regular renewals and terminations and does not total 100% because pending applications are not shown.
Frequently asked questions
When does Medicaid expansion end?
There isn't an end to Medicaid expansion. Once a state has expanded the income criteria for Medicaid, the new rules stay that way. States can choose to pass a law changing the Medicaid eligibility rules back to before it was expanded. However, no states have done this because it would mean fewer people can afford health insurance coverage. States that haven't expanded Medicaid can decide to expand at any time.
Did N.C. expand Medicaid?
Yes, North Carolina expanded Medicaid, and more people became eligible for coverage on Dec. 1, 2023. You're now eligible for Medicaid in N.C. if you earn less than $1,800 per month as a single adult or less than $3,697 per month as a family of four. As of January 2025, about 610,000 people have signed up for Medicaid because of the new income eligibility rules.
What is a Medicaid redetermination date?
A Medicaid redetermination date is your deadline to reapply for Medicaid to show that you're still eligible. You'll usually get a letter a month or two before your Medicaid redetermination date telling you that you need to complete a Medicaid renewal form. This form along with any requested paperwork, such as pay stubs or tax returns, needs to be submitted before your redetermination date. If you miss this deadline, you'll lose your Medicaid and will have to reapply, which can take a few months to get coverage again.
Why are people losing Medicaid in 2024?
A lot of the 11% drop in Medicaid enrollment in 2024 is because of Medicaid unwinding. That means people have to reapply for Medicaid coverage, while during the pandemic they could keep the coverage continuously. However, some of the drop in Medicaid coverage is also because of regular Medicaid cancellations and issues with applications.
Sources
- Medicaid.gov
- Data.Medicaid.gov
- Kaiser Family Foundation
- N.C. Medicaid Expansion Dashboard
Editorial note: The content of this article is based on the author's opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.